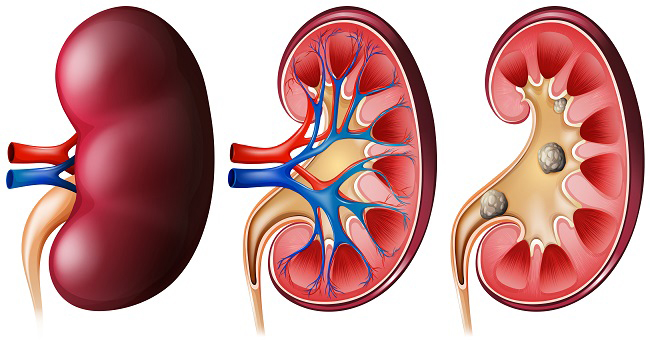
It is common knowledge that diabetes can damage many organs in the body including the kidneys. Kidney function is very important for a person’s well-being and hence scientists have constantly been searching for ways to protect the kidneys in diabetic patients.
A recent clinical study has found that a type of medication used to treat diabetes may have additional health benefits. This class of medication, called the Sodium-glucose transporter 2 (SGLT2) inhibitors, has been shown to increase uric acid excretion and decrease blood uric acid levels in patients with diabetes who have normal kidney function. Both these effects can help to protect the kidneys from the harmful effects of diabetes.
Diabetes is a condition that happens when your blood sugar (glucose) is too high. It develops when your pancreas doesn’t make enough insulin or any at all, or when your body isn’t responding to the effects of insulin properly. Insulin is a naturally occurring chemical substance in the body that helps to keep blood sugar levels normal.
Many drugs are used to treat diabetes. These include insulin for type 1 diabetes and oral blood glucose-lowering drugs for type 2 diabetes. However, the harmful effects of diabetes on the kidneys are a particular cause of concern and there is a need to develop treatments that can prevent this damage.
A recent clinical trial has explored the use of drugs called SGLT2 inhibitors for protecting kidney function in diabetic people.
The clinical study, published in the Clinical Journal of the American Society of Nephrology, analyzed data from 54 patients with Type 2 diabetes who were given an SGLT2 inhibitor, either dapagliflozin or empagliflozin. The medication works by blocking a protein called SGLT2, which helps the kidneys reabsorb glucose back into the bloodstream.
The researchers found that treatment with dapagliflozin or empagliflozin resulted in an increased loss of uric acid in the urine as well as a decreased blood uric acid level. Uric acid is a waste product of protein breakdown that is normally excreted by the kidneys, and high levels of uric acid in the blood have been linked to kidney damage including kidney stones.
Hence, by increasing the loss of uric acid and by decreasing the uric acid blood levels, SGLT2 inhibitors protect the kidneys from the harmful effects of diabetes.
In conclusion, this clinical trial highlights the protective effects of SGLT2 inhibitors on kidney function in people suffering from diabetes. It emphasizes that this medication is a safe and effective option for diabetic people.
If you have Type 2 diabetes and normal kidney function, talk to your healthcare provider about whether SGLT2 inhibitors may be a good treatment option for you.
__________
Clinical Journal of American Society of Nephrology, May-22
About Diabetes
Innovative Clinical Trials Study New Treatments for Diabetes
Diabetes Clinical Trial Gave Me a Fearless Life
Managing Depressing in Type 2 Diabetes with Melissa Officinalis Extract
The Impact of a High-Fiber Diet on Type 2 Diabetes
Multicomponent Healthcare Intervention for Glycemic Control in Type 2 Diabetes
The Potential of Sleep-Opt-In for Type 1 Diabetes Management
Efficacy of Dorzagliatin as an Add-On Therapy in Diabetes
Benefits of Advanced Hybrid Closed Loop System for Type 1 Diabetes
Intermittent Fasting Shows Promise in Managing Type 2 Diabetes with Insulin Treatment
Clinical Trial Shows How to Reduce Risk of Kidney Stones in Diabetes
Clinical Trial Confirms the Link Between Obesity and Diabetes
Innovative Clinical Trials Study New Treatments for Diabetes
Medical Breakthrough for Type 1 Diabetes Patients
Could a Simple Blood Test Predict Diabetes?
About Diabetes
Innovative Clinical Trials Study New Treatments for Diabetes
Diabetes Clinical Trial Gave Me a Fearless Life
Managing Depressing in Type 2 Diabetes with Melissa Officinalis Extract
The Impact of a High-Fiber Diet on Type 2 Diabetes
Multicomponent Healthcare Intervention for Glycemic Control in Type 2 Diabetes
The Potential of Sleep-Opt-In for Type 1 Diabetes Management
Efficacy of Dorzagliatin as an Add-On Therapy in Diabetes
Benefits of Advanced Hybrid Closed Loop System for Type 1 Diabetes
Intermittent Fasting Shows Promise in Managing Type 2 Diabetes with Insulin Treatment
Clinical Trial Shows How to Reduce Risk of Kidney Stones in Diabetes
Clinical Trial Confirms the Link Between Obesity and Diabetes
Innovative Clinical Trials Study New Treatments for Diabetes
Medical Breakthrough for Type 1 Diabetes Patients
Could a Simple Blood Test Predict Diabetes?
