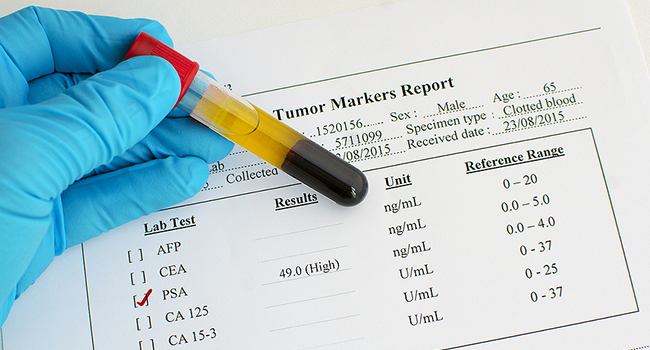
Prostate cancer affects men, with over one million new cases diagnosed yearly. One way to detect prostate cancer is through a blood test that measures the levels of a protein called prostate-specific antigen (PSA) in the blood. While PSA screening can help reduce prostate cancer mortality, it can also lead to the overdiagnosis and overtreatment of low-risk cancers.
Clinical Trial
In a study, researchers evaluated the incidence of prostate cancer among men with PSA levels below 3 ng/mL and no prior prostate cancer diagnosis. The study followed the men from their first PSA screening attendance and ended with a prostate cancer diagnosis, emigration, death, or the study's closing date.After a median follow-up of 17.6 years, the cumulative incidence of prostate cancer was 9.1 % among men with PSA levels below 3 ng/mL. The incidence was 3.6 % for men with PSA levels between 0 and 0.99 ng/mL, 11.5 % for men with PSA levels between 1.0 and 1.99 ng/mL, and 25.7 % for men with PSA levels between 2 and 2.99 ng/mL. The study found that the risk of prostate cancer increased significantly as PSA levels increased, particularly for low-risk cancers based on the Gleason score and the European Association of Urology (EAU) risk group.
The study suggests that men with PSA levels below 1 ng/mL have a low risk of developing clinically significant prostate cancer over 20 years. In contrast, men with PSA levels between 2 and 2.99 ng/mL have a much higher risk, with a 4- to 5-fold increased risk of developing aggressive prostate cancer.
